Black fungus: Outbreaks of deadly fungal infections might sweep the world

In India, against the backdrop of a powerful wave of COVID-19, thousands of cases of mucormycosis, a dangerous fungal disease, are recorded. In severe cases, doctors remove the eyes and parts of the face to save a life. The infection is difficult to treat due to anti-fungal drug resistance. Who is at risk, and whether it is worth fearing illness?
We are surrounded by millions of microbes. We breathe in, eat, carry viruses, bacteria, moulds on our skin. They are not dangerous for a healthy body, but an invisible enemy attacks as soon as it fails. Fungal infections are especially insidious: they are asymptomatic, difficult to treat, usually lasting for months, and have severe side effects.
It affects people who already have serious health problems: HIV, cancer, organ transplantation, diabetes, extensive wounds, burns. The mortality rate for fungal invasions is very high.
Mucorous fungi, candida yeasts, and aspergillus moulds are pathogenic. Although some of their representatives are useful in science, medicine, as well as in everyday life – they are used in experiments as test organisms, as leaven, to obtain antibiotics.
They live in the soil, on sick plants, on the walls of rooms with high humidity, and form fluffy colonies on various plant substrates. The fungi reproduce by microscopic spores, from which mycelium (fungus) and hyphae grow, drawing water and nutrition from the environment.
In 2009, a previously unknown species of the pathogenic fungus Candida Auris was isolated from the ear of an elderly woman with otitis media at a hospital in Tokyo. Similar cases were later confirmed in 15 other patients. Candida Auris became an extremely aggressive pathogen, resistant to many medications, and contagious. Its origin and natural source have not yet been determined.
The infection quickly spread around the world. In 2017, it was first diagnosed in a hospital in Florida (USA), and exceptional measures were taken to prevent its spread: even contacts of those infected were monitored. During the pandemic, patients with COVID-19 were admitted to the hospital, and in July 2020, four cases of Candida Auris were detected among them.
All patients were tested. Of the 67 people in the covid ward, 35 were found to have antibodies to the pathogen. Eight died within the next month, but it is impossible to say what the contribution of the fungal disease was there. Scientists believe that the germ was spread on staff clothing and mobile medical equipment that had not been properly disinfected.
For the first time, the fungus Candida Auris was identified in 2009 in Japan. Since then, it has spread throughout the world. In the United States, the number of cases grew from year to year. Against the backdrop of COVID-19, new outbreaks are expected.
A double epidemic in India
Mucor fungi have been known since the 19th century when they were isolated from sick animals. They live in soil, plants, manure, on rotting fruit. It is encountered by those closer to the ground, for example, dogs, which are constantly sniffing everything.
Mucormycosis occurs as a complication of chemotherapy. Usually, if the patient’s blood count is below a critical level, anti-fungal therapy is started to prevent it. However, particularly insidious germs bypass it. Then the last resort is the bacteria-derived antibiotic amphotericin. The drug has the worst side effects, which is why medicine is in desperate need of new anti-fungal drugs and vaccines.
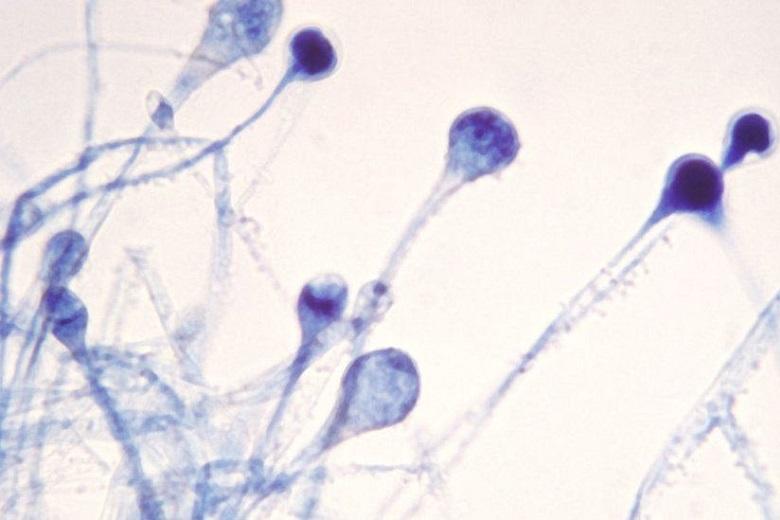
Mucor fungus spores enter the nasopharynx, settle in the sinuses, proliferate, produce hyphae, and produce toxins that degrade tissue and bone. Visually, the hyphae are black in colour, hence the name of the disease, black mould. The infection enters the skull, blocks major arteries and veins, and causes bleeding.
Before the pandemic, mucormycosis in humans was extremely rare. However, there was a real outbreak in India against the backdrop of the powerful wave of COVID-19. Two hundred thousand new cases a day are detected there.
The explosive growth is attributed to a special Indian variant of coronavirus. Fungal infection in patients discharged or on the mend is superimposed on this. More than half of exotic disease cases occur in the western states of Gujarat and Maharashtra.
Since it is very difficult to recognize mucormycosis on its own, people come to doctors with advanced forms when immediate surgical removal of tissues, eyes and jaws is required. Otherwise, the mortality rate is almost 100 per cent.
Many people attribute the mucormycosis outbreak to the use of steroids in the therapy of severe COVID-19 patients. These anti-inflammatory drugs actually save lives but suppress immunity. Unlike Candida Auris, mucormycosis is not transmitted from person to person or from an animal – you can get it from the environment by breathing in the spores. Perhaps ventilators and oxygen use contribute to the infestation. But these are just theories.
It is no coincidence that India finds itself at the epicentre of a dual viral-fungal epidemic. In countries with tropical climates, the concentration of spores in the environment is immeasurably higher than in the temperate zone.